Our vision for MSK
We aim to help transform musculoskeletal care in the private sector. We’ve been working with specialists and the healthcare services designer HBS UK to build services that focus on patients' needs.
We also want to improve patient access to healthcare services providers who are suitably equipped to meet their clinical needs.
Our current muscles bones and joints service already directs AXA Health members to appropriate care.
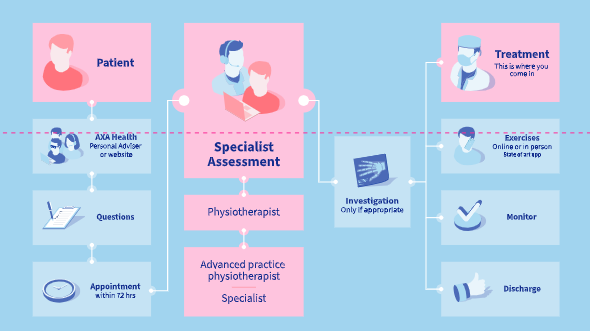
We now want to take this further, ensuring that a suitably qualified healthcare professional speaks to the patient at the outset of their treatment journey. To do this we’re working with HBS UK and its MSK services platform (see below).
MSK care re-imagined
At the beginning of the healthcare journey, HBS UK's Lucy platform deploys
- a specialist-designed triage questionnaire
- online assessment of the patient by a healthcare professional experienced in musculoskeletal medicine
- and includes online access to diagnostic investigations where appropriate.
Referral stage
At referral, the platform
- hosts online consultations and
- holds the electronic patient record.
This approach improves speed of access and efficiency of referrals for treatment, ensuring patients are referred to a suitable practitioner in a timely fashion. It also creates a better patient experience and offers secure, centralised record keeping.
Features
The features of the platform, designed by clinicians, include:
- standardised triage questionnaire. Devised over several months by a multi-disciplinary team of orthopaedic surgeons, rheumatologists and advanced practice physiotherapists. HBS UK reviews the questionnaire as part of a continuous improvement process.
- patient history: designed following standard clinical procedure.
- clinicians carrying out the initial assessments are peer selected and peer reviewed, with substantive NHS posts and private practice experience
- diagnostic investigations are ordered according to clinically evidenced protocols
- three software updates for the platform are issued each year.
Results
HBS UK reports that the first 8,000+ online assessments gave early PREMs and PROMs data which are extremely promising.
For example, PREMS scores of the treatment experience, in a population of 2,300 patients seeing a specialist, advanced practice physiotherapist or physiotherapist, averaged 4.6 on a five-point score for first appointments and 4.5 for follow ups (figures drawn from quarterly report covering June/July/August 2021).
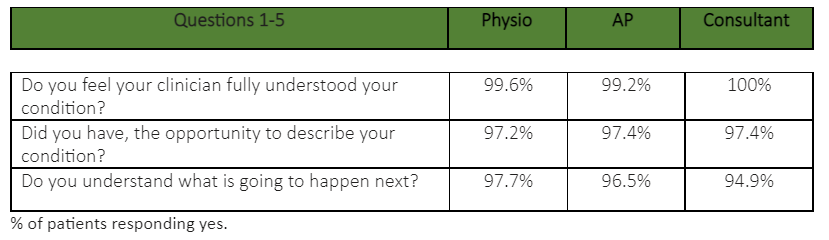
Below are some of the questions and responses expressed as percentages.
Pathway
What our members say


More efficient referrals
Academic poster analysing the efficiency gap between referrals made via the HBS UK-managed pathway and the traditional referrals model (i.e. GP to specialist).

How we refer patients to you
These are the guidelines we follow when referring patients to providers.

Working with the body
Our existing muscles bones and joints service directs members with MSK conditions to the appropriate healthcare provider
- Members worried about symptoms call us
- Phone assessment with physiotherapist
- Members directed to self-care, physiotherapist treatment or consultation (and possible treatment) with specialist.
Transforming MSK: a webinar from AXA Health and HBSUK
In spring 2021 some 160 orthopaedic specialists attended a webinar hosted by AXA Health and HBSUK to discuss how the Virtual LucyTM service aims to transform musculoskeletal healthcare for AXA Health members.
Speakers were Sarah Taylor, AXA Health Head of Specialist and Practitioner Relations; Fergus Craig, AXA Health Commercial Director; Mr Mark Emerton, HBS UK CMO; Lucy Cassidy, HBSUK Head of Service & Design and Charles Byrne, HBSUK MD.
For more information, please see the questions answered below, or email AXA Health Specialist Account Manager Emma Harris: emma.2.harris@axahealth.co.uk.
The following similar questions were submitted on the subject of fees:
Q: Are the specialist consultation fees unchanged from existing AXA agreements?
Q: Will AXA be paying their recognised consultants more for helping to deliver this high-quality service?
Q: I presume there will be a different scale of fees if seeing patients through this pathway?
Q: As this reduces the number of patient encounters for a consultant and only provides you with patients who have failed conservative measures; is this then associated with increased reimbursement fees?
Q: [Is there] any difference in fees?
Q: What [is] the likely impact on remunerations?
Q: Will this change the fee structure?
Q: Still need to know the impact on fee scales for OP referrals - new and follow-up.
Q: Seems inevitable that clinicians will earn less as one less consultation before diagnostics.
Answer for all questions: there will be no change at this time to existing initial and follow-up fees for patients seen in-person on the Virtual Lucy pathway.
Q: Will clinicians have to pay to use the platform?
A: There is no charge for using the system at this stage for AXA Health members.
Q: Is AXA thinking to develop a "direct line" for this group of consultants to streamline referrals?
A: If this relates to direct booking into face-to-face clinics, this is something we are exploring and would welcome the opportunity to discuss with any of you how we could make this work most effectively.
Q: Will a patient’s BMI be available at first assessment?
A: Currently no, this information is not captured, but it has been discussed as a beneficial feature for the future.
Q: Is there any potential for the specialist to interact with the physio/AP the patient has seen previously? Questions regarding type of rehab and response? Or is the pathway a one-way street with no route back through rehab if the patient/specialist decide further non-surgical management is appropriate?
A: At the moment, there is no two-way communication possible, but we are looking at this potential.
Q: How have issues of institutional bias such as clients with language issues [been] addressed with this system?
A: We are looking at healthcare inequalities, including literacy and language with the NHS and AXA Health.
Q: Is the direction of travel that all AXA patients will need to use Virtual Lucy at some point in the future?
A: AXA Health is moving to a multi-channel service so there will always be choice for members in how they access care. Virtual Lucy will, though, replace our current direct access service run by physiotherapists over the phone.
Q: Does the referring clinician have access to feedback on their referral?
A: Not at this stage but the system will continue to develop richer MI to enable continuous improvement of the service to patients.
Q: I see a large number of patients who are given incorrect or inadequate physio exercises. As a result, I show the exercises in clinic and very rarely need physio at all. How do I do that through the platform?
A: We believe there is an opportunity to manage and monitor evidence-based physiotherapy programmes through Virtual Lucy. At the moment, the exercise programmes can only be generated from the initial assessment, but we are keen to look at integrating further to assist the face-to-face elements if we can.
Q: I'm trying to work out how to incorporate consenting in my practice, I would like to see AXA support clinicians and agree a fee for consenting clinics.
A: We are investigating this at the current time.
Q: [Firstly] is it possible to import the images from your CIMAR into the hospital I am seeing the patient in? This is important for review of images in our MDT. Secondly, I usually have preferred radiologists who understand what I am looking for and report my scans. Is there any scope for offering preferred radiologist for scans?
A: Yes, CIMAR is a universal PACS accessible from most UK private hospitals. The imaging centre is driven by patient choice, in the main if they have a local imaging centre they would probably use this. However, if they chose to have an image away from their home location, the radiologist at this site would have provided the reporting.
Q: I work closely with our MSK radiologists and discuss complex patients before and after scans. Will there be the ability to discuss scans/reports with the radiologist?
A: It is likely that the scans will have been done in the same hospital that you work, but if not, the report attached will give details of the reporting radiologists and you are always welcome to contact them.
Q: If a patient has imaging in NHS, will that be available, with imaging and report?
A: Yes, the patient can upload any previous image or report into the system.
Q: Imaging is not one size fits all, who decides on what imaging is required, what happens if I feel the imaging is not adequate?
A: Second images can, of course, be ordered at the discretion of the clinician and then patterns like this will be monitored to improve the service.
Q: Are we able to refer for further diagnostics if needed, e.g. if a patient has had an MRI but needs an MRI arthrogram am I able to refer for this?
A: Yes.
Q: I usually [to] weight bearing X-rays of foot. Is it possible to influence this so that I do not have to repeat the X-rays?
A: Yes, this is available for the requesting clinician.
Q: Does this risk over-investigating patients? Easier to avoid an MRI if a patient is examined rather than seen virtually.
A: The intention is quite the opposite, it measures this routinely and feeds back to clinicians so they can see their clinical ratios including their propensity to investigate.
Q: When are the referrals to specialist going to start?
A: The service is already live.
Q: Will you be recording the consultations the patient has over Virtual Lucy?
A: Yes, all consultations are recorded and kept for 7 years.
Q: How is the outcome data processed - is it accessible by us as clinicians?
A: At the moment, the Accelerated Assessment Data is available to HBS and AXA Health from the system. Reports can be developed to feedback to clinicians.
Q: I am interested in the 72 hours to see a specialist. If my clinic in a particular hospital takes place every Wednesday, what happens if the patient calls on a Thursday?
A: The 72 hours is for a Virtual Lucy appointment, not a physical one.
Q: How large a geographical area can you refer on to? I work in the middle of nowhere but at a tertiary referral centre that takes patients from all over the UK.
A: We refer across the whole of the UK.
Q: How long do you anticipate a new appt will take, including time to review delivered imaging and clinical review notes (and make patient feel heard, consent them for surgery etc)
A: A triage appointment is allocated 20 minutes on the system - there is no limit placed on your own face-to-face appointments as there is no interference with your own clinical practice or judgement made by this system.
Q: How do the face-to-face appointments get booked to see the specialist? Through the private hospital clinic booking service?
A: Via AXA Health customer services.
Q: Will there be an electronic version of the referral for the consultant?
A: In due course yes, but initially the system sends a message to AXA Health customer services to book an appointment and it arrives manually. An email to the practitioner is sent securely with a copy of the letter attached and a link to the image.
Q: I attended the meeting in London, when it was said that the first Consultant assessment will happen in a predetermined time slot that I have to provide. Is that still the case?
A: Yes, and whilst the volumes are at their current levels, we appreciate that this is difficult. That is why we are working to increase the volumes.
Q: If people choose to be seen by a sports physician and subsequently have surgery through a second referral, would they be registered as a double / inappropriate referral as their pathway was confounded?
A: No, if this is patient choice and is clinically appropriate for the patient. However, this is something we will monitor.
Q: Do you know where we practise?
A: Yes, but to be certain we'd recommend you keep your account on The Private Practice Register up to date.
Q: Will you be writing to us to formalise this arrangement with those of us who choose to go ahead with this?
A: Please see relevant questions in the 'Specialist practice section' or email emma.2.harris@axahealth.co.uk with any questions.
Q: How is the consultant appointment booked? Via consultant secretary or an online booking system?
A: Currently via your secretaries, by AXA Health’s customer service, in the same way as all referrals. However, we are really interested in an online booking solution. We would like to hear what works for them.
W: If we do this as active participants, is this something I am expected to fit into my normal clinic or are we going to run this at a separate time with a dedicated virtual Lucy clinic? We all have embedded systems and I am considering the added work I would need to do for a Virtual Lucy patient.
A: If you are receiving face-to-face referrals these would be booked in your standard clinic time. If you are wishing to participate in the remote assessment team, then you will need to allocate some time. For further information, please email onboarding@hbsuk.co.uk.
Q: Will all clinicians using the patient have access to relevant data, i.e. if patient has seen a physio or sports medicine person before seeing me?
A: Yes, the data from the initial assessment will be included in the referral letter from the triaging clinician.
Q: I am also assuming [that] the logistics of when I do this clinic, duration of the clinic, etc. will be discussed before starting the clinic. How will I be informed that there is an appointment booked for me?
A: Please contact onboarding@hbsuk.co.uk if you are interested in being a part of the triage team; otherwise no changes will be expected to your current practice, other than that you will, as a preferred specialist, receive more referrals.
Q: How do I know I'll be able to review the pre-consultation clinical management in my hospital-based clinic room, i.e. do individual private hospitals have to give permission for software to be downloaded or would I need to bring my own laptop to my clinic?
A: This is a web-based portal; as long as there is adequate Internet connection there shouldn’t be an issue, however we recommend you check for local firewall restrictions.
Q: If a referral is made to a consultant from a physio, will that appointment be treated as an initial or a follow-up consultation?
A: Any referral to an in-person clinician from triage will start as an initial appointment.
Q: Do the patients go back into the virtual follow-up post surgical intervention, and are outcomes/PROMs data collected on results?
A: No, once the patient is referred to a treating clinician, care is the responsibility of that clinician. As a question to us we will still ask the members to upload PROMS, so we will inadvertently be collecting overall outcome data. PROMS are collected at 0, 6 and 12 weeks.
Q: How will the patients be sent for assessment and who assesses? My worry is that this may lead to assessment by less than the best and more investigations.
A: The pathway is designed so that the patient is assessed by the most appropriate clinician the first time.
Injections/remote appointments
Q: Will your APP's be administering injections?
A: No - all appointments are remote (via telephone or video call).
Q: Steroid injections for OA: when you say you will have exhausted conservative management; I hope that doesn't mean everyone will have had a steroid injection. I know it's still in NICE guidelines but there is significant evidence now that relief from a steroid action is short acting and there are significant downsides: acceleration of disease, subsequent increased risk of infection at TJA.
A: All appointments are remote (via telephone or video call).
Patient choice
Q: Does the patient select the consultant or HBS clinician does?
A: Virtual Lucy shows options for the patient and the patient selects - but those options are only from an AXA Health list of preferred consultants.
Q: Please could you comment on how / whether this system might affect the individual patient's right to see the consultant of their choice?
A: Patients are not forced to use the system and as long as their policy allows, they will always be able to opt out and see their preferred consultant.
Q: How does the patient decide who to see?
A: For the onward referral following the Virtual Lucy assessment, patients will be offered all clinicians who have clinics close to the patient (work or home).
Q: Will patients be seen via this procedure or can they ask to be seen face-to-face?
A: We are offering choice so some members who have seen their GP may want to see a consultant in-person. This option remains but will be outside this pathway. You will continue to see referrals via the traditional route but also by this route too if you sign up.
Q: When the patient clicks to see a specialist post rehab, I presume Sports and MSK consultants will be available in the option lists for the patients under "knee" "shoulder" etc.?
A: Yes.
Right clinician
Q: Fast is not always the wisest. Getting to right is the most important.
A: This service does not interfere with the current practice of consultants in any way. If there are further improvements which can be made further down the line, we will obviously be keen to discuss those with the group This service is about getting people to the right care as quickly as possible, not just about speed.
Q: I am interested in the 'patient relationship' which develops after seeing a patient a couple of times - especially for more significant surgery - they might want to see us more than once - for an operation - a big investment in emotion for many people.
A: Once a patient is referred to you for face-to-face treatment, you treat them as standard. We are not looking to change the patient / specialist relationship.
Right treatment
Q: My experience is that a diagnosis is often delayed when a patient meets a physical therapist with an MRI scan before they meet me, an orthopaedic knee / hip surgeon. I believe in many instances the MRI report is treated and often leads down the wrong avenue especially where the knee condition is not traumatic. What are your thoughts and are you auditing final diagnosis versus MRI report diagnosis?
A: All of our assessments will be routinely audited which is one of the main advantages of having such readily available data and MI reporting. We do empathise with this view, hence why we are using the platform to get the person to the right place as quickly as possible; and that could be a specialist.
Q: If a diagnosis is made without the patient having been examined, how do you guard against treating the scan not the man?
Q: How can virtual consultation help confirm the diagnosis other than order some investigations and decide treatment based on investigations rather than clinical examination?
A: Any investigation results are combined with the clinical history and assessment findings of the accelerated specialist assessment. Together this can be utilised objectively to determine an appropriate course of initial rehabilitation. If patients don’t respond as expected, then they can be referred onto a specialist, but no surgical intervention will ever be recommended or undertaken without the operating consultant doing their own physical assessment.
Q: How can the clinician be certain that the previous conservative management has been optimal? There are large variations in physiotherapy practices for different conditions, driven by correct diagnosis for a start, and then awareness of the evidence.
A: This is a very valid question and there is currently no way to determine this on a national level. As Virtual Lucy is collecting data on patient satisfaction and outcomes which are matched to any treating clinicians, over time we will start to build a picture of the most effective clinicians and be able to drive patients to the best services.
Patient experience
Q: What are the advantages of this approach compared to the traditional pathways in your view?
A: Recent surveys indicate that patients really like the speed of access and the ease of the system. We also believe the up-front questions tend to improve the quality of the consultation as many of the preferred questions (designed by an MDT of 100s of consultants and APs) will be answered by the patient prior to the assessment.
Q: The issue that I have had with remote triage in the past is that the patient attends preprimed with the expectation of an operation. This can then be difficult when surgery is not the best option.
A: No patients are told what to expect from this Virtual Lucy service.
Right diagnosis
Q: Very few cases am I able to be sure of the diagnosis on virtual consultation.
Q: The biggest drawback of virtual consultation is lack of clinical examination. How could MSK be sure of their diagnosis with virtual consultation?
A: Virtual consultations will always have limitations, but on many occasions the clinical history is often paramount, and it can be used to determine if any likely surgical intervention is required. If the triaging clinician feels the patient needs a clinical examination, they will of course refer onto a specialist for a face-to-face appointment. There will of course be variations between specialities and suspected pathologies. The accelerated specialist assessment is to determine appropriate next steps and of course a lot of patients don't need to see a consultant but need rehabilitation.
Q: How are patients virtually examined to distinguish those with a grade 4/5 power vs 3/5 power (footdrop vs non-footdrop)?
A: Someone with a foot drop would be referred on for face-to-face assessment. There is no change to the receiving consultant's own practice.
Treatment plan and current practice
Q: Is the referral, after triage, still 'as usual', giving us the opportunity to see a patient more than once for assessment of progress and discussion of surgical risks - e.g. seeing a knee replacement twice before surgery - and is invoicing for these patients as per our standard fees - sometimes innovations come with a price pressure...?
Q: Are you saying that you will have decided the patient requires treatment? What if I do not agree with your treatment plan?
Q: A question for further down the patient pathway. Consent for surgery should not be at initial consultation or day of surgery, by default therefore an additional clinic appointment for consent is required, this should be a chargeable appointment. Please comment.
Q: I’m a spine surgeon, it can be clear from the referral that an MRI request is likely, however the information needs to be sense checked. if I see a patient and then suggest an MRI and then see again at the end of the clinic I can’t bill for new consultation and fu consultation, discouraging a one-stop patient pathway. Please comment.
A: This service does not interfere with the current practice of consultants in any way. If there are further improvements which can be made further down the line, we will obviously be keen to discuss those with the group.
Q: It is imperative we move to [a] digital booking.
A: This service does not interfere with the current practice of consultants in any way. If there are further improvements which can be made further down the line, we will obviously be keen to discuss those with the group.
Working relationships
Q: We often have close relations with radiologists and physios who we trust and respect. Does this take away some of that? Can we preserve it? Paid re-recording? Further physio under a known physio?
A: This pathway does not take away from any existing relationships and you are free to continue to work with radiologists and physios in your network. It is most likely that the investigations will have been done in the same private hospitals as your clinic, so the same team you know and trust.
Conversion rates, feedback, fees
Q: Do we get FB for our appraisal?
A: At the moment, the Accelerated Assessment Data is available to HBS and AXA Health from the system. Reports can be developed to feedback to clinicians.
Q: Will the higher conversion rate expected not negatively impact the perceived and currently analysed conversion rate for surgeons?
Q: One of your criteria for preferring specialists is conversion rate - which I assume means you like a low conversion rate. But with Virtual Lucy we have a higher conversion rate. so no longer preferred?
A: We recognise that, as we are triaging and sending you appropriate patients for this cohort, your conversion rate will be higher.
Q: As a clinician seeing patients through the Lucy pathway I will have to assess, interpret imaging and counsel the patient regarding treatment. This would usually be spread over two consultations. Has AXA considered the extra appointment lengths needed and time pressures on our clinics.
A: At the current time the fees remain unchanged at the NP rate.
Access
Q: I am assuming we need the software installed to use this system?
A: No, it is web-based.
Q: Can clinicians access the online portal from their own laptop?
A: Yes.
Q: Is this web-based app also MAC applicable?
Q: Will this work well with MAC?
A: Yes, this is accessible with a MAC device.
Imaging
Q: Is it possible to import the images from your CIMAR into the hospital I am seeing the patient in? This is important for review of images in our MDT.
A: Yes, CIMAR is a universal PACS accessible from most UK private hospitals.
Q: Can we upload the imaging to our hospital system, as [we] will need for it to be up in theatre etc..
A: Images can be downloaded from Virtual Lucy PACS viewer as DICOM files which can then be uploaded into any local systems.
Dictation
Q: Can you dictate into Virtual Lucy using Dragon dictate?
A: Practically yes, you can dictate into the fields on Virtual Lucy.
Q: Is there any option to attach a clinic dictation at the end of the consultation and get it transcripted in 24 hrs? The transcript can be sent to the clinician [for] get it checked and a copy of this can then be sent to the patient, GP and clinician records.
A: Not in this iteration.
General
Q: Can you link with DGL?
A: There is currently no interoperability in place with other systems but the system is capable of interoperating with any web-based system. These changes will be further down the development roadmap.
Q: Can we download or print for our own records?
A: Yes.
Joining the triage team
Q: How do we sign up to join the panel of virtual experts?
A: Please contact onboarding@hbsuk.co.uk.
Q: What would the remuneration vs time spent mean for me were I to join the triage team? I’m already keen to sign up to receive referrals.
A: Please contact onboarding@hbsuk.co.uk for details.
Q: What [is] the format of the triage clinics is and what the pay for it is?
A: Please contact onboarding@hbsuk.co.uk for details.
Selection for the triage team
Q: What is the process of the triaging consultant selection: is it by invitation or some other process?
A: Application and approval.
Q: Does AXA select which consultants will be on triage team?
A: No, but they are AXA Health-recognised specialists.
Q: How are ‘specialists’ selected? As a fellowship trained knee surgeon, I only offer knee related appointments. Is this recognised?
A: All the HBS team are peer-reviewed sub-specialists.
Q: So, no consultants who don't have NHS appointment involved?
A: If consultants have retired from an NHS substantive position, they are welcome to join the triage team and receive referrals as long as they are recognised by AXA Health.
Q: How does the skill set of the HBS UK Specialist Team consultants compare to the consultants taking the final specialist referral? Are they more generalists then sub-specialists? Can individual consultants be in both groups? If so, would they have to see first referrals outside their primary specialty area?
A: All the HBS Team are peer-reviewed sub-specialists. Yes, they can be in both groups. No, they wouldn’t have to see referrals outside their primary specialty area.
Q: Who is triaging the patients?
A: Advanced physiotherapists or specialists.
Q: Who is the triaging clinician? Physio or Orthopaedic Consultant?
A: Both, plus sports medics and rheumatologists, the choice depends on the answers to the initial questions.
Q: Where does sports medicine / MSK physicians fit in with Virtual Lucy?
A: There are sports medics on the triage team already.
Q: Not sure who you are seeking to be triage assessors? Is this work for MSK physios or consultant surgeons or both?
A: For both.
Q: Which specialists have been chosen to be a triage specialist and what is the remuneration ?
A: They are AXA Health-recognised specialists that HBS have chosen based on sub-speciality.
Q: What do you want from us as clinicians - do you want us to sign up as treating specialists or do you want us to sign up for the specialist assessment service, or neither, as we are already recognised as AXA specialists?
A: One of the purposes of this session was for attendees, if they haven't already done so, to sign up for receiving patients via Virtual Lucy. If you want to join the triage assessment, please contact onboarding@hbsuk.co.uk
General
Q: If I am on the triage team as a consultant, and a consultant provider of treatment, what are the rules around referring patients onwards? Can I refer a patient to myself?! Or do triage clinicians do their triage work for patients outside of their geographical area?
Q: If you can triage and see pts too, are they totally independent of each other?
A: There is nothing in the rules stopping you referring to yourself if you are on the the local options for a patient. These things will obviously be monitored and measured but the opportunity to do so will be relatively rare.
A: How many hours would you need for triage care a week? Or is it by case by case basis? What time of the day could I run the triage if asked to do so?
A: It’s entirely at the discretion of the individual consultant.
Q: For those virtual triage consultants seeing the patient first - who is providing the indemnity insurance for this work?
A: Their own MI companies, following individual discussion.
Q: [Wasn't] the virtual fracture clinic conceptualised and started in Glasgow?
A: The first Virtual Fracture Clinic in England was in Brighton at the same time as the Glasgow system was developed.
Q: I have issues with being described that 'surgeons' are only interested in undertaking the surgery, I have to disagree that Consultants are by far the best diagnostic persons!
We are not describing surgeons as only interested in undertaking surgery, this is why we have created an MDT
Q: When HBS UK reached out in 2020 to enlist consultants for the triage team, their signup process seemed to be quite onerous, including documentary evidence etc. which may have put some of us off. Could these details not have been transferred across from AXA records?
A: Practising privileges are not the same as PMI recognition so unfortunately governance dictates that a 15 to 20-minute online sign on process is necessary.
Q: How will you build the clinician 'Bio'?
A: There is a standard template for completion for the Virtual Lucy system for the clinician to complete.
